Instability of the lumbar spine - information, diagnosis and treatment
There can be many different reasons for lumbar spine instability to occur. Nevertheless, the most common reason is the natural degeneration of the spine. Instability of the vertebral column means that within the corresponding movement segment there might possibly be abnormal mobility. Long-term, the compensatory mechanisms of the spine cannot counteract this abnormal mobility. Over time, a deformity occurs and as a result the patient experiences severe back pain. Treatment is initially conservative. However, if during the course of the treatment an increase in deformity or pain is noted, a surgical stabilization is necessary to restore the segment's original position.
How do we define "instability"?
"Instability" means that the spine as a result of everyday physical stress cannot maintain its original mobility causing the nerves to degenerate and also causing a more extensive deformation or severe pain (Panjabi and White).
What are the causes for an instability of the lumbar spine?
During the aging process, wear and tear occurs throughout the body, the spine is not exempt from this process. This development follows a certain pattern:
- Initially, the discs gradually lose their ability to bind water. As a consequence, they cannot adequately cushion the loads on the spine, e.g. function as shock absorbers, and additionally they become thinner. They also bulge backward into the spinal canal.
- The loss of height of the intervertebral discs also means that the paired-scale facet joints slide into one another like a telescope. In this process the load on the facet joints is increased and the joint capsules become less flexible. In addition, the cross-sectional area of the nerve exit holes decreases, so that the outgoing nerve is constraint.
- As the intervertebral disc continue to lose volume, the stabilizing ligaments of the spine slacken, e.g. become less flexible. To be mentioned here is primarily the yellow ligament, which stretches between the individual vertebral arches. By approaching the adjacent vertebral arches, the yellow ligament bulges into the spinal canal and narrows it further.
- The combination of these changes finally results in the motion segment consisting of two vertebrae and the intermediate disc, yellow ligament in instability. This instability causes back pain. The body now does something very useful - it tries to stabilize the unstable motion segment again. It achieves this by growing bone. The result is that bone braces are formed between the adjacent vertebrae, which eventually cause the segment to stiffen and the instability pain to subside. We sometimes refer to this process as the "blessed stiffening of the age".
Given these conditions, there may be two scenarios that determine the person concerned to look for help from a spine specialist:
- The instability of the lumbar spine is so strong that the body is not able to stabilize the motion segment itself by growing bones and / or the body has genetically only a very low ability to grow the necessary bone. In this case, “repair” of the instability by the own body is not possible. Consequently, the deformity of the spine and the back pain is increases and nerve damage may develop. At this point, the spine surgeon must perform the necessary “stabilization” of the motion segment.
- The body is able to stabilize the motion segment, but the instability pain caused by this process is extremely strong and cannot be controlled by the conservative treatment, e.g. pain relievers and injection therapies. In other words, the person concerned cannot be expected to wait for improvement that might occur in the natural course of his disease. Again, the spine surgeon must decide in favor of his patients and perform surgical stabilization of the motion segment affected.
How is instability of the lumbar spine diagnosed?
Typically persons affected by the disease, report that they feel like their back is “braking apart”. A thorough physical examination of the spine will indicate to what extend an instability is present. A confirmation of the physician’s diagnosis is obtained by an X-ray of the lumbar spine from the front and laterally. This method allows assessing the shape of the spine, and a displacement or a rotation of two vertebral bodies to each other is easily recognized. Functional images, i.e. a lateral radiograph in forward and reverse tilt of the trunk, will show the instability more clearly. Magnetic resonance imaging (MRI) completes the imaging. With the MRI, the physician can assess the length of the vertebral canal, the condition of the intervertebral discs and facet joints as well as the state of the back muscles.
What are the treatment options of an instability of the lumbar spine?
The first choice is a conservative therapy, which includes mainly physiotherapy in order to strengthen the back muscles. Physical measures lead to a relaxation of aching back muscles. Pain and anti-inflammatory drugs are administered. Injections in the facet joints relieve the back pain, injections into the spinal canal (SSPDAs) sooth irritated nerve roots. X-ray examinations of the lumbar spine should be performed for early detection to avoid an increase of instability.
A surgical stabilization is indicated when:
- paralysis in the legs occurs caused by nerve damage;
- a conservative treatment of a duration of six to eight weeks is not a resounding success and back pain still persists;
- the instability is increasing according to the X-ray follow-up and at the same time the pain has not subsided;
- The instability is from the outset pronounced in such a way (e.g. a very pronounced spondylolisthesis) that the conservative treatment does not seem to be successful.
Whenever a surgical stabilization is planned, the first step is always to perform a so-called "segment diagnostics”. In rare cases only one of a motion segment is affected, usually several segments are worn. To make sure that the correct segment is stabilized, injections specifically targeting the small vertebral joints are used. When an injection alleviates the pain, the spine specialist knows that it is this segment causes the pain and that after a stabilization an improvement of back pain is to be expected.
 What are the procedures of a lumbar fusion surgery?
What are the procedures of a lumbar fusion surgery?
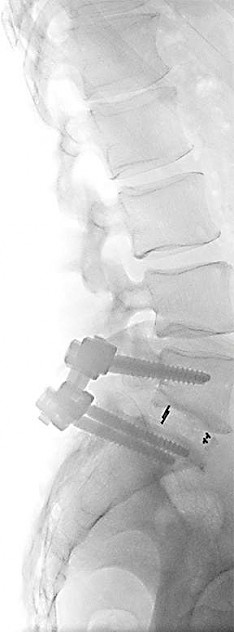
In the "Posterior Lumbar Interbody Fusion” (PLIF) the surgery is performed from the back (posterior). In the the affected vertebral disc above and below, two screws are inserted respectively. The screws are then connected on each side by a metal bar.
The spinal canal is now being extended posterior by the removal of the vertebral arches to eliminate bottlenecks. Then, the disc is removed from both sides. In place of the discs two placeholders made of plastic (so-called "cages") are now placed between the vertebrae, which restore the original disc height and bending of the disc.
The "Transforaminal Lumbar Interbody Fusion" (TLIF) is an alternative to PLIF and is also performed from the back (posterior). The great advantage is that this operation can also be performed minimally invasive with several small incisions. This protects the overlying back muscles, which must not be dissected from the vertebral arch. The plastic placeholder is placed only on one side between the vertebrae. Now, a bar is attached on both sides of the screws.
The TLIF is a muscle-sparing surgical method that the spine surgeon performs to stabilize a lumbar segment if a) there is no significant spinal stenosis and b) no extensive repositioning maneuvers are required.
The "Anterior Lumbar Interbody Fusion" (ALIF) is performed from the front and is the method used when surgery of the back (dorsal) cannot be performed. In the ALIF a less invasive method is selected by accessing the spine through the abdominal wall musculature, in which no muscle should be severed. Now an intervertebral disc can easily be removed and a placeholder made of plastic ( "cage" ) is inserted.
After a lumbar fusion surgery, the patient can leave the bed the first day after the operation. The patient learns techniques that allow him to move the back without causing damage in the first few weeks after surgery. Sitting is immediately possible. Step by step, the patient regains normal mobility and independence. After about seven to ten days, the patient can be discharged from the hospital. Following the surgery, further stabilizing by means of outpatient physiotherapy should be performed in order to strengthen the core muscles.

