If no tumor cells are found in the biopsy, but the PSA value remains high, prostate carcinoma cannot be ruled out with certainty. Therefore, the first step is to conduct a detailed interview and clinical examination of the patient to look for other possible causes of the elevated PSA levels. These include, for example, mechanical stress on the prostate caused by cycling or inflammation of the organ.
However, if the suspicion of prostate cancer remains, the current guidelines recommend a repeat biopsy within 6 months. Prostate biopsy is an established and safe procedure and is currently the only way to definitively diagnose prostate cancer.
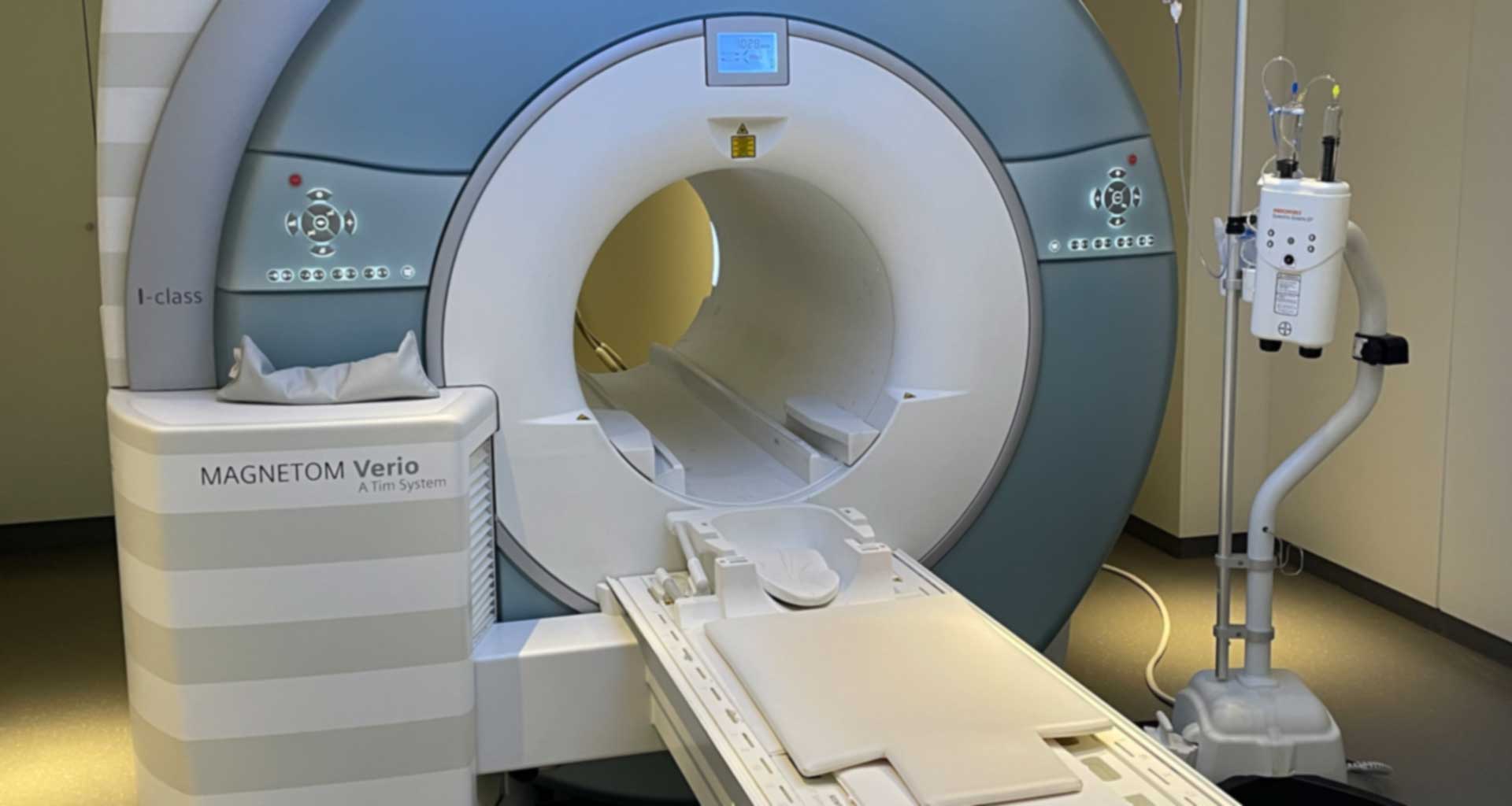
However, in order to improve the detection of a possibly existing prostate carcinoma after negative tissue sampling, the West German Prostate Center uses the so-called MRI-assisted biopsy. Prior to the actual tissue removal, the patient's prostate is scanned in a special magnetic resonance imaging (MRI) scanner, the so-called multiparametric 3 Tesla MRI. This creates a kind of "map" in which areas suspected of having a tumor are marked, which the urologists then use to orient themselves precisely when removing the tissue. The actual biopsy then takes place in a second step under the control of a high-resolution transrectal ultrasound. By combining both diagnostic procedures, we increase the hit rate and can thus spare the patient possible further biopsies.